Raven asked a good question in comments:
I don’t understand that privatized Medicaid stuff — what value do the care management firms add? But they do take a cut…
This whole idea that a business bureaucracy is somehow more cost-effective than a government bureaucracy strikes me as a load of bullocks. What’s the business model — underpaying the office staff?
Mayhew Insurance has a Medicaid managed care organization (MCO) contract. I have spent quite a bit of time in the past two years working on MCO projects, so take that as you will.
What is the value proposition for a state to go the MCO route?
I see several.
- Cost predictability
- The ‘Bob’ or the external evil bastards
- Preventative care improvements
The first is an MCO structure gives the state way more cost predictability. MCO’s are paid a capitated rate per member per month. Membership will be divided into different categories (Medicaid Expansion populations, long term disabled, maternity, poor kids) where the rate is different but the MCO bears the risk. The only risk that a state budget bears in a given year is the number of people who sign up for Medicaid and a bit of case mixture (a lot more kids signing up is a lot cheaper than a lot of long term disabled adults newly signing up). The MCO’s take on most of the medical cost risk.
If there is a 300 person knife fight at the National Hemophiliac Association’s Medicaid task force session, the MCO(s) covering those individuals pays to stop the bleeding, not the state.
Over the course of several years, the value proposition of this risk shifting is fairly low. If an MCO has to pay for the fight at the National Hemophiliac’s Association conference in Year 1 and incurs massive losses, the state will send higher risk adjusted rates to that insurer in the future to make them close to whole again. The biggest value is the MCO reduces payment variability from the state. Variability is expensive as surprises are expensive.
Secondly, MCO’s are great evil bastards. An MCO like Mayhew Insurance can say “No” to individuals and they blame us for being evil, soulless, money sucking bastards. Politicians can call our C-level folks into meetings and yell at them on cable access TV. This is important for the cost control that is needed for most state budgets to work.
For instance CVS is a major pharmacy benefit manager (PBM). They are restricting a dermatological cream for toenail fungal infections. Currently that cream costs $1,000 a bottle before discounts. CVS is probably receiving a bulk discount of 25% to 50%. Right now, Jublia could be prescribed as a first choice medication. CVS will be restricting Jublia as a last chance medication. People will be required to use other, less expensive anti-fungal creams to see if they work first. If they don’t work, CVS will approve Jublia. This is an explicit cost control step. However Mayhew Insurance which uses CVS as a PBM, are the evil bastards telling people no instead of the state government.
Again, this is not a good economic value proposition, but MCO’s are effectively being used to outsource blame and tough decisions that imposed by a strong budget constraint.
The final and good reason to use the MCO model is that it seems that the MCO’s do a better job of getting people preventative care and screening. This makes sense. State fee for service systems are optimized overwhelmingly to pay claims quickly and cheaply. They are not optimized for intensive care management as that is just net new spend within a single budget year. The MCO’s make money in two ways on Medicaid contracts. The first is to spend less money on net than the capitated payments. Preventative care such as flu shots averts hospitalizations. This is one of the reasons why MCO’s are aggressive in flu vaccine outreach. It leads to direct in-year cost savings. Secondly, most states with an MCO model have preventative care bonus payments built into contracts. MCO’s tend to better at getting preventative screening.
Michigan Medicaid has a good example. I’ve been following the Flint lead crisis. One of my first thoughts was where was Medicaid screaming about lead poisoning. Below is a marked up slide from the January 2013 Michigan Medicaid overview:
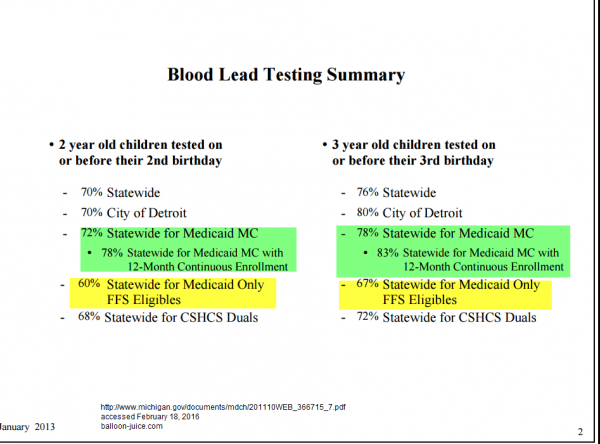
The MCO’s had a significantly higher screening rate than fee for service. This is a notable example because of the wider Flint lead poisoning crisis, but it is a common scenario. The MCO’s do add some value in better preventative care than traditional fee for service arrangements.

Revrick
Richard, you and Charles Gaba (aka Brainwrap) are founts of knowledge, wisdom and understanding when it comes to health insurance and related issues. Thank you.
OzarkHillbilly
Nice to know it’s not all about privatizing profits while socializing risks. Thanx for the bolts (I already have the nuts, I live in the hill country)
Barbara
This is a large question, but I can tell you that one thing private contractors do better than the government is to experiment about finding what works and to ditch what doesn’t. They also maximize the collection and use of information in making decisions. For instance, a private insurer will typically know about drug and hospitalization trends within a matter of days or weeks that the government won’t figure out for two years. This is attributable in part to the bureaucratic procurement and budgeting process, which limits the degree to which public officials can decide to do something or expend resources just because it makes sense, much less impose costs on others with political clout. Whereas, this is the essence of a private business model. These limitations are perhaps essential in a large bureaucracy, but they do have adverse consequences when it comes to large and complicated and fragmented programs like Medicaid or Medicare. I have known of several really serious and well-thought out demonstration projects that were completely stillborn because the government could not, literally, provide data in a timely fashion that was necessary to make them work. You can’t reduce unnecessary hospitalizations if you don’t even know someone has been hospitalized until six months after they were released. So the government tends to use blunt force measures, like penalizing hospitals for readmissions instead of, like a lot of private insurers, sending case managers to the hospital to try to determine the appropriate length of stay and make sure after care service needs are being met. But the effect of the penalty is the same: to push down onto a private actor the incentive to engage in experimentation to see what works in preventing readmissions. Another thing the private companies do in Medicaid is create accountability (for them) for access to care, which doctors and hospitals don’t, mostly because of their own political clout. IMHO, people tend to have an inflated opinion of the efficacy of the fee for service Medicare program, in particular. It’s incredibly fragmented and no one has an incentive to coordinate and save you time and effort, and of course, not money.
Richard Mayhew
@Barbara: I’ve had issues getting good and timely data from governmental entities, and I’ve had issues getting data from privately owned provider entities even though those assholes asked us to conduct an analysis on their covered population but could not supply non-claims data for that fucking project.
Big entities that don’t think in data are a pain in the ass without regard to who signs their pay checks.
JCJ
So the “death panels” are staffed by the personnel at Mayhew Insurance. Has anyone told Sarah Palin?
Richard Mayhew
@JCJ: 2nd Floor mainly, they are great to get coffee with but don’t eat the almond tort as that is where they hide the cyanide
Lee
I’m probably showing some ignorance here but I’ll ask anyway. My guess is the answer could be a post in itself.
So was Medicare Advantage basically one of these just with Medicare?
If so, wouldn’t these also eventually have the same issues?
Karen
Richard, I just got off the phone with a billing company for the rehab I went to last year to help me walk. I was on Medicaid and and MCO last year yet I keep on getting bills that from different providers through their billing companies. So far I’ve been calling them and inform them I don’t owe them because I was on Medicaid and giving them my MCO’s address and ID# and my Medicaid ID. Can you please tell me if I’m handling this right? Thanks!
Barbara
@Richard Mayhew: A lot of health plans institute “prior authorization” for hospital stays simply to make sure they know who is in the hospital, not necessarily to micromanage care. But my biggest laugh is over hospitals that argue against having to notify insurers within one business day that someone has been admitted because it’s too hard to keep track of people. Is that supposed to be a point in their favor? That it’s too hard to keep track of who is actually there?
Barbara
@Karen: It’s the right thing to do but it would be better to follow a phone call up with a written statement in case they start trying to sic collection agencies on you. As a Medicaid beneficiary, your liability for “balance bills” is extremely limited.
Barbara
@Lee: Medicare Advantage only covers Medicare benefits, but lots of people are eligible for both Medicare and Medicaid (“dual eligibles”). The difference between MA and a lot of Medicaid initiatives can be described like this: The agency that oversees it is highly motivated to protect the Medicare population, and correspondingly not motivated by the prospect of simply saving money. There are states that have the same attitude toward Medicaid managed care, like California, but many states see Medicaid managed care solely through the lens of cost containment. My mother has an MA plan and she loves it. She likes it much better than having to figure out Medicare fee for service on her own.
Roger Moore
@Barbara:
Your legal liability may be limited, but that won’t keep them from trying. Good luck getting your money back if you don’t know your rights and are intimidated into paying.
Barbara
@Roger Moore: Totally agree. I have fought this fight and it saddens me to know how much people lose solely because they do not understand their rights.
Richard Mayhew
@Karen: Sounds like you are handling this right… if they keep harassing you, start writing down every phone conversation with real time notes, get name/identifier info, and forward to your state attorney general and let them know that you are doing so.
Alex
@Richard Mayhew I’d like your perspective on Michigan’s (currently rather vague) proposal to replace the public MCOs that currently provide Medicaid behavioral health services (Community Mental Health) with private HMOs. The CMH PIHPs already get a capitated rate to smooth out costs, and assume the associated risks. And they already manage cases preventatively. The main argument for replacing them with HMOs seems to be that it will integrate behavioral health and developmental disability (capitated Medicaid) with physical health (fee for service Medicaid). The goal is to save $ and get better outcomes. But why wouldn’t the PIHPs be able to do that, too, for lower overhead? We are talking about the most complex, expensive cases imaginable; none of the HMOs contracting with Medicaid in Michigan have expertise with this type of thing. And HMOs in general don’t have a great track record on handling behavioral health– they were only recently mandated to cover it.
Richard Mayhew
@Alex: That is a level of detail where I have no relevant knowledge. I don’t know enough about Michigan and I don’t know enough about the behavioral health side of the business to have an intelligent conversation about either.
Ohio Mom
Anecdotes not data but we have Medicaid as a secondary insurer for our kid and I am very happy I deal with Medicaid directly. It seems enough to deal with one commercial insurer, who I swear is currently trying to shift all the cost of son’s recent tonsillectomy onto Medicaid by doing things like alleging the hospital coded the surgery as needed for obesity and they don’t pay for tonsillectomies to treat obesity. No you nitwits, it’s for the obstructive sleep apnea that was diagnosed through the sleep study you paid for, use some common sense.
So I get to make calls to the hospital, asking them to check what codes were submitted, and I get to call the insurance company and ask them questions like, “Why aren’t you paying for the visit to meet the surgeon before the operation, wouldn’t it be terrible medicine to skip that step, you couldn’t have possibly meant to do that.”
I can’t imagine having another entity in the mix. I didn’t know I had that to be thankful for but now I am filled with gratitude.
JCJ
@Richard Mayhew: Thanks for the advice! Too bad. I like almond torts.
Jacel
Thank you for this explanation. I wouldn’t have known what value (other than grift) this arrangement had, but you make plausible points. Also, thank you for the knee-slapping “knife fight” example in your explanation.
Richard Mayhew
@Jacel: One of my long standing “other duties as assigned” tasks has been to come up with very odd corner cases to test out models.
I have the National Hemophiliac convention knife fight as a stress tester for reserve accumulation (it is an 8 sigma event in most scenarios, so we’re fucked)
I have the medical effects of the Battle of Hogwarts as another scenario plus a zombie outbreak and what happens iof all ambulance drivers drive like an 83 year old grandmother who needs a nap.
Those are fun to write up.