Jerry asked an awesome question yesterday in the discussion about how medical spending fell off the cliff in the first quarter:
How would this scenario have changed if we were under an M4All system? Or would answering that question require a whole book to answer?
We need to define a critical term first — Medicare for All is a payment system. It determines who pays for care (the federal government mostly with some patient level cost-sharing).
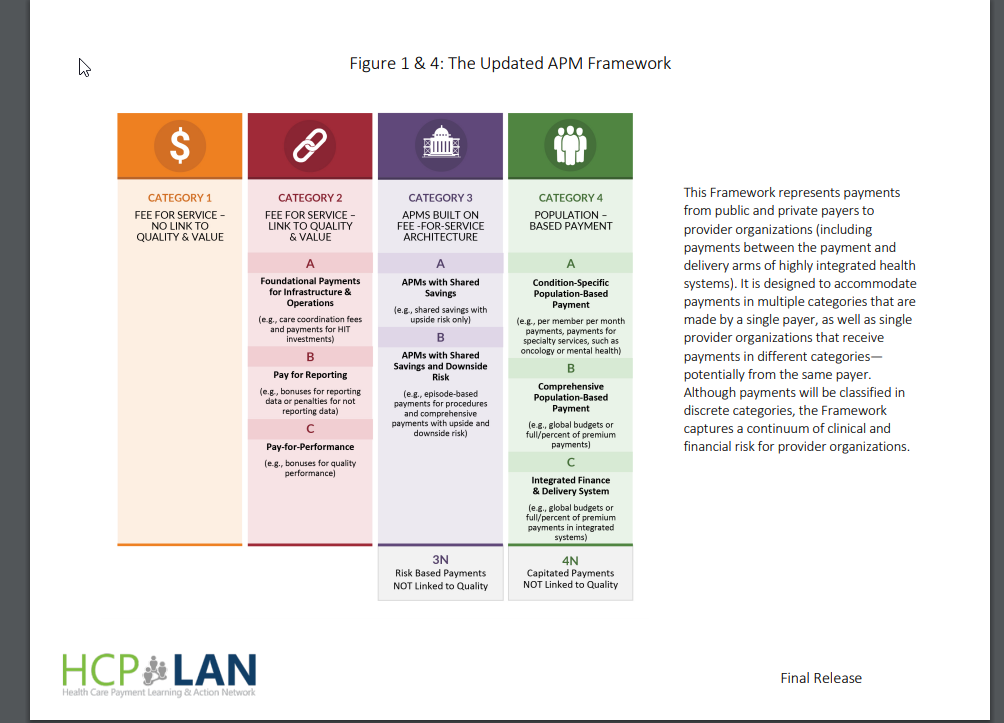
The critical question is how is payment made by whomever is paying for medical care. I will be massively oversimplifying things but there are basically two extremes on the continuum of payment systems. The first is fee for service. Here the clinicians get paid for each thing that they do. They replace a knee, they get a check. They diagnose kindergarten crud as a typical and benign virus, they get a check. They intubate and care for someone in the ICU with COVID, they get a check. I am wrapping up a lot of complexity here as I am including bundled payments, prospective payment systems for Medicare based on diagnosis groupers and true fee for service into this conceptual bundle but the core element is payment is driven by a patient receiving a service and payment levels for any particular provider is determined by the number and types of services provided.
The other extreme of the payment end is population level payments and global budgets. These can be condition specific or general. In these payment systems, the payments are made on a regular basis without regard to the actual utilization. Clinicians receive a per person per month (PMPM) payment. If the doctors/hospitals spend more in a month, the clinical group loses money. If the doctors/hospitals spend less than the payment, the clinical risk holder makes money.
Under this system, revenue would see far less of a drop for clinicians receiving capitated global payments. Revenue could drop from ancillary services and from carve-out payments that rely on fee for service, but revenue under a global budget system if far less elastic to circumstances than fee for service systems.
So the fundamental question that needs to be asked is not who is paying (Medicare for All vs. Blue Cross + UnitedHealthcare + Centene + Medicare + Cost-sharing etc) but how payments are made (Fee for Service vs the continuum of global budgeting).

Baud
This seems bad for the patient.
David Anderson
@Baud: Any payment system, if taken to a logical extreme has bad outcomes for patients.
Bob Hertz
I have been reading about global budgets ever since Drs Woolhandler and Himmelstein brought them up back in about 1989.
I always thought they were pie in the sky, basically because no federal authority could reach an acceptable allocation of funds.
However, the current experience may open a window for this rational method of funding hospitals.
David Anderson
@Bob Hertz: ACOs and the Maryland Hospital Global Budget and Pennsylvania Rural Hospital experiment are all variants on global budgeting.
Bob Hertz
@David Anderson: I am not sure that the Maryland system is full global budgeting. For example, Johns Hopkins has been suing patients who do not pay their bills.
In true global budgeting, there are no hospital bills. The hospital lives on its annual allocations.