Maryland is making a big push to increase health insurance coverage in the state. There is a recently signed bill that dramatically lowers the friction to enroll. Stan Dorn, one of the architects of the policy proposal, has more at Health Affairs:
the Maryland Easy Enrollment Health Insurance Program (MEEHP)….represents the country’s first attempt to use income tax filing as an immediate on-ramp to health coverage. By simply checking a box on their state income tax return asking the exchange to determine their eligibility for free or low-cost insurance, an uninsured tax filer can have relevant information from their return sent automatically to Maryland’s health insurance exchange. The exchange then uses that data and other available records to determine the individual’s eligibility for Medicaid, CHIP, and PTCs….
People who qualify for Medicaid or CHIP are invited to choose a managed care organization by a specified date. If they neither choose a plan nor opt out of coverage, they are enrolled in a Medicaid plan by default….
Uninsured tax filers with incomes too high for Medicaid or CHIP have a brief special enrollment period (SEP) for enrolling into the individual market. The SEP is triggered by the filing of a return with the relevant box checked, so long as the return is filed before a date specified by the exchange (presumably April 15 or earlier). The exchange determines PTC eligibility as quickly as possible, encouraging uninsured consumers to obtain insurance and helping them select an appropriate plan.
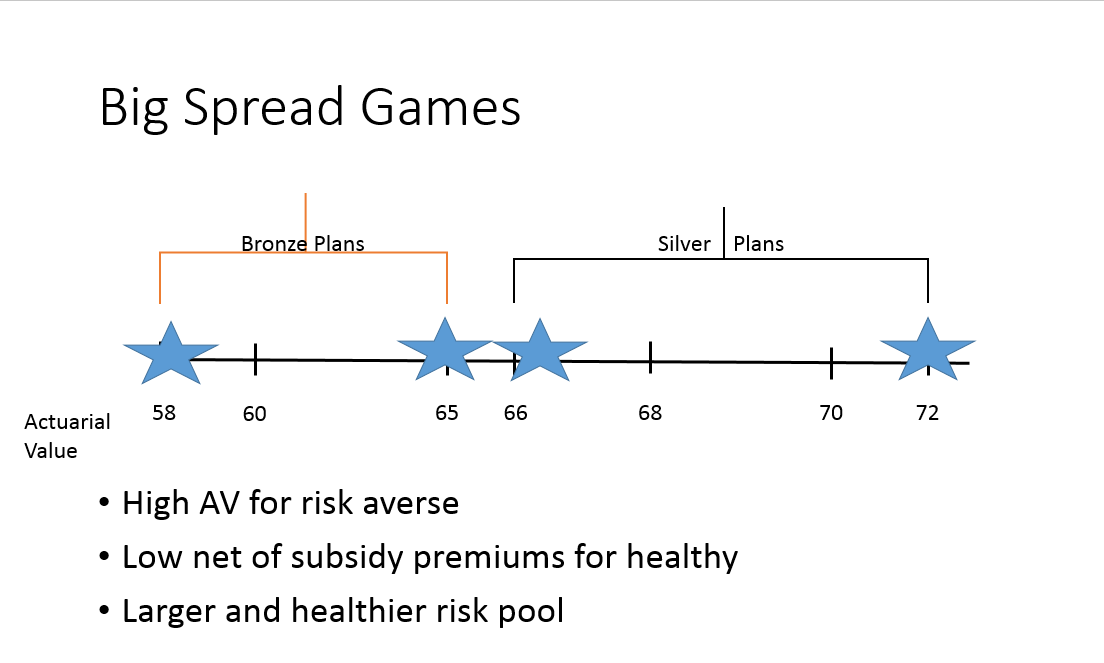
The default assumption in Maryland is that people want to be covered and the state government as well as the Exchange board should facilitate that coverage using current data streams. Eyeballing 2019 data on RWJF Hix Compare, most single 27 year olds earning under 180% FPL will be exposed to at least one zero premium Bronze plan. Older buyers and larger families will see zero premium plans at higher income levels. Some families will see zero premium silver and gold plans.
Facilitating on-exchange enrollment is a net positive for the state as it will increase the number of people covered and most likely decrease the average morbidity in the pool. It is the easier step as it costs the state a slight increase in administrative costs but no program costs. The federal government takes on the entire incremental cost of increasing on-Exchange enrollment if that enrollment is exclusively coming through zero premium plans.
More notably is the commitment by Maryland to expand their Medicaid rolls. Medicaid has split financing; some state and some federal. Depending on the type of eligibility an individual has, Maryland is paying anywhere from ten to fifty percent of the incremental costs. We saw with the launch of the ACA exchanges that there was a significant “woodworker” effect as people who were always qualified for Medicaid actually enrolled in Medicaid as health insurance coverage had higher salience. We should expect a similar, but smaller, woodworker effect as Maryland uses its administrative systems to maximize enrollment.
Maryland is adding lubrication to the health coverage system while many other states are throwing sand to increase the friction people must fight through to get and maintain coverage.
Reducing enrollment frictions in MarylandPost + Comments (7)