Attribution is the process of assigning patients to groups.
This matters today because we have engaged in a decade long practice of attempting to transform care delivery in the United States by creating a proliferation of Accountable Care Organizations (ACO). An ACO is a clinical entity (a hospital system, a collection of physician groups etc) that agree to take a per-capita payment for a group of patients and gets a bit more flexibility to organize and administer their care. An ACO can profit if total cost of care at a given quality level comes in under the target. An ACO can lose money if total cost of care is over the target. The ultimate payer, such as the federal government for Medicare ACOs, can share some of the savings and losses.
One of the key questions in any ACO is who is the ACO responsible for? This is the attribution process. There are a lot of attribution algorithms out there that can split a universe of patients into groups of (ACO A, ACO B, not assigned) pretty well. However, one of the key questions is when does the ACO get the final list of patients it is financially and clinically responsible for? There are two choices. Retrospective attribution looks at the care performed on patients during a performance year at the end of the year. Attribution is based on who the ACO actually sees during the performance year. The finalized list is given to the ACO after the contract year is over. Prospective attribution looks at the care performed on patients prior to the start of the contract year. The ACO gets the final list on the first day of the contract year.
These are big choices to make. Prospective attribution will, by definition, miss people who move into the area or join the program for the first time in the performance year. Retrospective attribution will include people on the list who received care from the ACO provider network in the prior year but moved three time zones away at the start of the year, but the ACO is still responsible for their costs.
In a new paper at the American Journal of Managed Care led by Dr. Brystana Kaufman, a Duke Margolis colleague and friend, in work funded by the Gordon and Betty Moore Foundation, we simulated attribution to ACOs that are already in the Medicare Shared Savings Program using both retrospective and prospective methods to look at the differences in attributed populations for Medicare ACOs among populations defined as “seriously ill”.
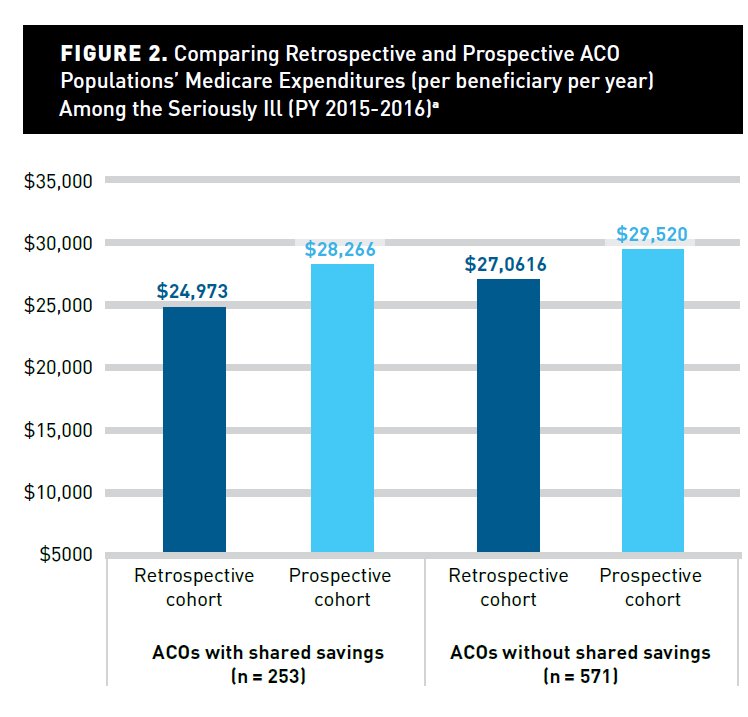
There are big differences depending on what method is used.
Retrospectively assigned cohorts are cheaper than prospectively assigned cohorts.
Why is that?
Dying in the first 90 days of the performance year was associated with reduced odds of retrospective ACO attribution (odds ratio [OR], 0.24; 95% CI, 0.24-0.25) relative to beneficiaries surviving 270 days or longer. Similarly, hospice use was associated with reduced odds of retrospective assignment (OR, 0.80; 95% CI, 0.79-0.80).
Retrospective attribution needs certain types of claims in the performance year. Dying in the first three months of the performance year makes it difficult for the right types and number of claims to accumulate. Hospice in Medicare also does funny things to claims accumulation. The lack of claims makes assignment of individuals to an ACO using retrospective attribution difficult.
Prospective attribution picks up the soon to be dead as people who are in the last chunk of their life are likely to have significant utilization in the last full claim year of life. And it is this last full claim year of life that prospective attribution is looking at to assign people to an ACO. A prospectively assigned cohort will have much higher first quarter mortality in a Medicare ACOthan a retrospectively assigned cohort just because of who is included in the assignable universe.
So what does this mean beyond a half dozen geeks geeking out?
We’ve identified the start of a business case for specific focus on serious illness. If we want to make serious illness care more central to ACOs, then our choice of attribution methods matters a lot. If we want ACO leadership to be concerned about how the last year of life is treated in an ACO, then prospective assignment gives a very strong financial motivation to redesign care around the needs of this population.
Furthermore, a recent change to the Medicare ACO program allows for an ACO to choose which type of attribution they want. Previously, Medicare used retrospective attribution. Now an ACO may be able to make strategic choices to select the type of population that they think they are better at serving. This could have federal fiscal impact without changing overall care quality or efficiency.


Another Scott
Interesting. But not really surprising, is it? Unless I’m misunderstanding, which is certainly possible.
Big picture:
1) Excluding people who immigrate and emigrate, if a person leaves one ACO and enters another ACO, then that cost is simply shifted to the other, isn’t it? So, as long as all the oldsters don’t move to FL and AZ, then one would expect the in/out motion to generally balance out if one does the averages appropriately, right?
2) How do the Retro/Pro averages work out on a per person per day basis (rather than a per person per year basis)? Is it significantly different? In other words, is the difference mainly the result of the Retro ACO being able to delay coverage for a significant part of the year?
Thanks.
Cheers,
Scott.
David Anderson
@Another Scott: Not massively surprising in the direction although we were surprised by magnitude.
As far as migration, it does not balance on net within a year. It mostly balance over time, but within year and therefore within management give a damn, a new arrival is outside of the ACO and not worth management attention while a departure is just a sucking chest wound of money.
It also assumes near equal migration in all directions and locations. I don’t think that applies as 68 year olds are far more likely to migrate to North Carolina from Michigan than vice versa.
SiubhanDuinne
Watching your boss (I guess?), Dr. Mark McClellan, on MSNBC right now.
David Anderson
@SiubhanDuinne: yep!
Omnes Omnibus
Is the fact that I saw ACO and immediately thought you had mistyped AOC a sign that I need a break from political blogs?
Barbara
This is the aspect of ACOs that, to me, dooms the whole project. Over time, if you look at the few ACOs that really seem to be successful, they all have one thing in common — they are organized and led by physician groups, not hospitals. Physicians know who their patients are, and they can direct them to tiered care options based on their condition. Hospital organized and directed ACOs, like hospital PHOs and HMOs and PPOs, usually exist for one reason, and that is to populate hospital beds. I know I am exaggerating, but not really by all that much.
egorelick
I do not understand the chart comparing MSPP ACO’s and non-MSPP ACO’s. What is it supposed to mean. Also, stupid question, but how do we know the entire result is simply not driven by the dataset that fails to capture end-of-life claims properly and, because of that, fails to properly allocate attribution? IOW, how do we know that a tweak (or even a more significant revision) won’t make this result disappear without any notice?
Ted Doolittle
I’m not opposed to ACOs, but I am uneasy. Like maybe, one out of three cheers.
I see the ACO project as really the centerpiece of the healthcare policy establishment’s program for the nation in terms of cost control — and that primacy is undeserved.
One of the main purposes, and maybe the key purpose, of ACOs is to save money. That’s the aspect of ACOs this comment is directed to.
A few things about them make me queasy:
Look, again, I’m not opposed to ACOs. Maybe they will work a bit. (And to be fair my comment here is limited to the cost/price side, not the quality side.) Maybe they are one arrow in our quiver. But ACOs won’t ever be able to make our healthcare system economically competitive. My concern is that the ACO effort has and will continue to suck time, energy, and brainpower from developing a real, brute-force, face-the-music, Sherman tank approach to the healthcare cost crisis in our land. If we want the same cost structures that our international economic competitors enjoy, better to try to import what works there (basically, public-private partnership in price negotiation) and bring it to our shores than to organically develop some novel strategy, shaped in good part by a felt need to conceal from patients and voters what is really going on, and hope that that will be enough.
Bottom line, ACOs … okay. Maybe nice to have, but too much fanfare, not that much beef, and at least so far crowding out and delaying the more difficult cost control debate we need to have.