Bob Herman of Axios was paying attention to the other important healthcare related CBO report yesterday:
There was another CBO health care release today. Similarly important/riveting. It's all about physician prices: https://t.co/ffUFwdQNt2
— Bob Herman (@bobjherman) June 27, 2017
This is an important report as it illustrates the spread between Medicare and Commercial rates. Unfortunately it does not have Medicaid managed care rates. With that limitation, this still provides a very good heuristic of thinking through the mechanics of how we pay for health care services.
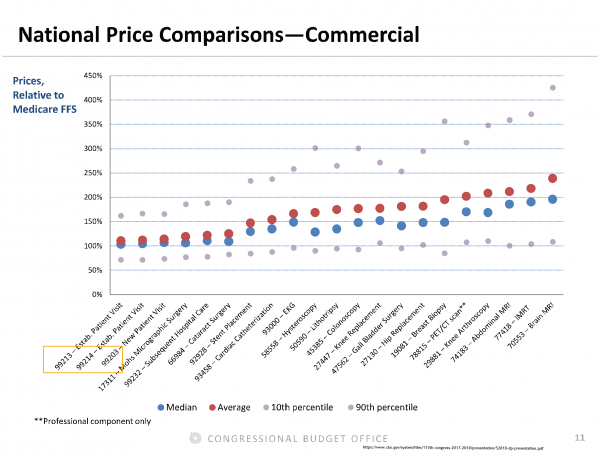
There are a few things to notice here. The first is that there is a wide variation of variance by type of procedure. The second is that of the five procedures that have the smallest median bump over Medicare rates, four of them are overwhelmingly procedure codes used by primary care physicians. We should want to use more primary care which means we probably should want to pay more for primary care.
The third point is that the heuristic that commercial payers pay about 50% more per service than Medicare is loosely supported by this chart. The details aren’t quite fine enough for that statement to be 100% certain, but it is a solid heuristic.
Finally, the most interesting thing to me are the trimmed ranges. The gray dots are the 10th percentile commercial payments and 90% percentile commercial payments. The 90th percentile for every procedure is very expensive. That is known knowledge and not particularly interesting to me.
More importantly, take a look at the 10th percentile. I am eyeballing the spread across 21 categories as being from about 70% Medicare rates for some PCP services to maybe 110% Medicare rates for imaging and orthopedic procedures. This is the business case for tiered networks, it is the business case for narrow networks, it is the business case for reference pricing. There are providers who are willing to take Medicare-like rates for common services. Engaging in any of the restrictive network or payment practices looks to exclude as many providers in the 90th percentile as possible while steering as much work as possible to providers who are willing to take near Medicare rates.
This is where money can be squeezed from commercial insurance where we currently pay way too much per unit of service. The downside of that squeezing is this means hospitals and doctors with local market power will be excluded from networks and services unless they drop their rates.

dr. bloor
Those imaging procedures should be low-hanging fruit.
David Anderson
@dr. bloor: Agreed. Should be, not sure why they are not in most circumstances
Juice Box
A lot of imaging procedures can be off-shored too.
japa21
IIRC, Medicare actually upped the PCP reimbursement a few years ago and slightly lowered others, particularly the surgical specialties. This was in response to the shrinking number of PCPs out there.
smintheus
The chart’s vertical axis is labeled
Does the acronym FFS mean what I think it means?
David Anderson
@smintheus: For Fuck’s Sake why aren’t you thinking about Fee For Service
smintheus
@David Anderson: I wonder if it has anything to do with uninsured people having a greater than usual propensity to pay for CTs and MRIs out of their own pocket? It’s often the first step doctors order, and won’t treat you further if you don’t. Once when I was without insurance I shopped around for a knee MRI, and the prices quoted varied astonishingly.
smintheus
@David Anderson: That’s what I was asking myself.
David Anderson
@smintheus: No, at least not in this chart. It is a chart of paid claims from Kaiser, UHC, Aetna and Humana vs. Medicare Fee for Service matched claims. It is only commercial covered claims in the data set that built this particular graph.
Sloane Ranger
O/T but related to this topic. CNN reporting that the Turtle has pulled the Bill as he didn’t have the votes. He is due to give a presser shortly.
Sabta xoneys
My father used to be a pathologist. In the mid 1960s he moved to Ohio and got a job at a hospital in his hometown. They paid him a salary. But by the terms of his employment he was required to belong to the county medical society, and their bylaws considered it unethical for a physician be paid a salary (i.e. not be paid by fee for service). They eventually worked it out, but I have been leery of physicians citing ethics or morals ever since.
Ohio Mom
@Juice Box: Maybe reading the imaging can be off-shored but I don’t have time in my schedule to go oversees for my annual mammo and DEXA. Not that I don’t enjoy traveling.
D58826
@Sloane Ranger:
From Huffington. But lets not pop the bubbly just yet. We have seen this movie before in the House. The moderates gave their blessing to a bill that was even worse than the original. Now while it wasn’t as bad the the Freedom caucus wanted, enough of the FC and the moderates voted for it to pass.
All this is really just a version of the old saying ‘Madame we have established what you are and now we are just haggling over the price’. We will watch a Yurtle haggles with a couple of his ‘madames’.
jl
Thanks for an informative post, and link to the CBO report (which I have already read through and saved). Provider market power in the US is not often mentioned in debates, though David Anderson has been talking about it on this blog for a long time. This might be hard to tackle because doctors are one of few professional groups in the US who have a good reputation. Attempting to grab high margin payers for the fat quasi-rents they will fork over is a big problem in the US. It’s also an emerging problem in the Netherlands, since their recent health care reform that makes the country a good comparison case to the US (that is probably the reason CA gub Arnold chose it as the model for his abortive attempt at health care reform in CA). In the Netherlands it comes from a different source, which is more vertical integration among providers from primary care through intensive tertiary care.
I think there are other mechanisms besides the ones discussed in the post. Stricter controls on physician and medical group self dealing is one. Reducing power of specialists in AMA in design of protocols and coding that favors specialist care. The AMA will have to forced or induced to do this, since they are a ‘reactionary’ organization (in scare quotes since I don’t mean politically but temperamentally). The are very reluctant to innovate anything in terms of business models or public policy, but then if it works for them they will be fine with it. Witness their switch on Obamacare, which is typical, IMHO.
Forcing price transparency in markets through a uniform tariff schedule for services, usually in terms of an allowable band of prices (which is far narrower in other countries compared to US). This approach is more common in Continental Europe where legal systems make it easier to implement.
timmeh
A small alarm always goes off for me is when they exclude Medicaid reimbursement rates which are at least 50% lower than medicare FFS for most codes. Medicare allows $98 for a 99213, medicaid pays $29. I know the ratio gets better on procedures, and procedures really are the place to bend cost, but when I see a graph like this, and imagine what I’d conclude if I wasn’t in the industry, I’m a little demoralized. We bust our humps to make accepting medicaid remain profitable, but if anyone was making decisions and excluding the burden medicaid-level reimbursement places on private practice, let alone hospitals, we’re gonna end up in an unsustainable place.
But maybe we run a diinosaur-era business model that needs to die off. Oh well.